
A pioneering review of knowledge on antimicrobial resistance and antibiotics in the environment
While antimicrobial resistance is a well-researched phenomenon in humans and animals, its dissemination in the environment is less well known. However, certain resistance genes that are currently a problem in medicine come from bacteria in the environment. ANSES was therefore asked to conduct an expert appraisal of the state and possible causes of contamination of aquatic and terrestrial environments in France by antibiotics, of resistant bacteria that are pathogenic for humans and of antimicrobial resistance genes. It also examined the mechanisms that promote the emergence and persistence of antimicrobial resistance in the environment.
This is one of the very first reviews of knowledge on this issue. To carry out its work, the Agency drew on the scientific literature and the results of research conducted in France on environmental contamination, in particular that funded by ANSES as part of the National Research Programme for Environmental and Occupational Health (PNR EST).
Contamination of the environment by antibiotics is due to human activities
Antibiotic concentrations in France are low, regardless of the setting. The antibiotics found most frequently in the environment are those that degrade the least, and are not necessarily the most widely consumed. The main sources of environmental contamination by antibiotics are related to human activities: discharges of treated wastewater and the spreading of sewage sludge and livestock manure. Antibiotics found in water are therefore in higher concentrations downstream of wastewater treatment plant discharges than upstream. There are fewer data on soil contamination, and these only concern agricultural spreading sites. The antibiotics and concentrations found depend on the spreading type.
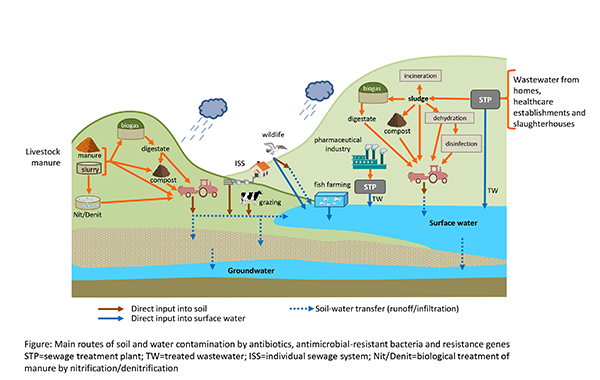
Main routes of soil and water contamination by antibiotics, antimicrobial-resistant bacteria and resistance genes
Resistant bacteria that disappear faster than genes
Antibiotics, resistant bacteria and resistance genes have the same contamination sources. Concentrations of resistant bacteria and resistance genes decrease the further they are from the source of contamination, whether this is a treated wastewater discharge or a spreading site. Although the treatments used on wastewater and spreading products can reduce the quantities of resistant bacteria and resistance genes released into the environment, they are not designed to eliminate them completely.
The antimicrobial-resistant bacteria studied are mainly of faecal origin. They have difficulty surviving in the environment and are mainly found at sites heavily contaminated by human activities. Resistance genes can persist longer, either outside cells or harboured by other bacteria not considered by the studies.
Study of the mechanisms that can promote the survival of resistant bacteria
ANSES's work also examined the environmental factors that may promote the selection of antimicrobial-resistant bacteria and the transmission of resistance genes. Few data are available on this subject. In general, it seems that the quantities of antibiotics found in the environment in France are too low to promote the survival of resistant bacteria and the persistence of resistance genes. In addition, their fate in the environment may be influenced by the presence of trace metal elements or biocides, the diversity of bacterial communities and the heterogeneity of the settings.
Improving the monitoring of environmental contamination and continuing to acquire knowledge
The results obtained are likely to evolve with climate change and developments in practices related to the circular water economy, such as the reuse of treated wastewater or artificial recharge of aquifers. These phenomena could indeed modify the routes of introduction and spread of antibiotics and resistant bacteria in the environment and affect its ability to dissipate this anthropogenic contamination.
To improve the comparison of data, ANSES recommends that all studies on antimicrobial resistance in the environment should monitor a set of indicators including several antibiotics, a specific resistant bacterium and a specific resistance gene. The Agency also suggests that these studies should take into account the fate of this contamination over time and spatially. Lastly, ANSES recommends consolidating and broadening current knowledge, whether on environmental contamination by antibiotics, bacteria and resistance genes, on the factors promoting their spread, or on the assessment of the ability of ecosystems to dissipate contamination.